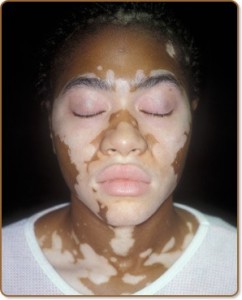
Vitiligo is a skin condition in which there is loss of pigment (color) from areas of skin, resulting in irregular white patches that feel like normal skin. It occurs when the melanocytes, the cells responsible for skin pigmentation which are derived from the neural crest, die or are unable to function.
Vitiligo generally appears in one of three patterns:
- Focal pattern — the depigmentation is limited to one or only a few areas
- Segmental pattern — depigmented patches develop on only one side of the body
- Generalized pattern — the most common pattern. Depigmentation occurs symmetrically on both sides of the body.
 In addition to white patches on the skin, people with vitiligo may have premature graying of the scalp hair, eyelashes, eyebrows, and beard. People with dark skin may notice a loss of color inside their mouths.
In addition to white patches on the skin, people with vitiligo may have premature graying of the scalp hair, eyelashes, eyebrows, and beard. People with dark skin may notice a loss of color inside their mouths.
The most notable symptom of vitiligo is depigmentation of patches of skin that occurs on the extremities. Although patches are initially small, they often enlarge and change shape. When skin lesions occur, they are most prominent on the face, hands and wrists. Depigmentation is particularly noticeable around body orifices, such as the mouth, eyes, nostrils, genitalia and umbilicus. Some lesions have hyperpigmentation around the edges. In regards to psychological damage, vitiligo can have a significant effect on the mental health of a patient. Vitiligo is associated with autoimmune and inflammatory diseases, commonly thyroid overexpression and underexpression.
There are a number of ways to alter the appearance of vitiligo without addressing its underlying cause. In mild cases, vitiligo patches can be hidden with makeup or other cosmetic camouflage solutions. If the affected person is pale-skinned, the patches can be made less visible by avoiding sunlight and the sun tanning of unaffected skin. However, exposure to sunlight may also cause the melanocytes to regenerate to allow the pigmentation to come back to its original color.
Home UVB narrowband phototherapy is a very common approach that treats vitiligo. The success rate is very high in children and in adults when the spots are on the face and neck. Exposure times vary; treatment frequency ranges from two to three times per week with a gradual increase in exposure every subsequent session.
About 0.5 to 1 percent of the world’s population, or as many as 65 million people, have vitiligo. In the United States, 1 to 2 million people have the disorder. Half the people who have vitiligo develop it before age 20; most develop it before their 40th birthday. The disorder affects both sexes and all races equally; however, it is more noticeable in people with dark skin.
Vitiligo may also be hereditary. Children whose parents have the disorder are more likely to develop vitiligo. In fact, 30 percent of people with vitiligo have a family member with the disease. However, only 5 to 7 percent of children will get vitiligo even if a parent has it, and most people with vitiligo do not have a family history of the disorder.
Management
There is no cure for vitiligo but there are a number of treatments available which can slow down or improve the condition. In fair-skinned people, avoiding tanning of normal skin can make patches of vitiligo much less noticeable. Treatment options generally fall into four groups:
Sunblock and other means to protect the pale skin
A high protection sun-block (factor 20 or above) is applied to areas of vitiligo to prevent sunburn. Affected areas of skin are protected when the sun is strong, especially in the middle of the day by wearing, for example, a wide brimmed hat and long sleeved clothing.
Skin camouflage
In mild cases, vitiligo patches can be hidden with makeup or other cosmetic camouflage solutions. If the affected person is pale-skinned, the patches can be made less visible by avoidingsunlight and the sun tanning of unaffected skin. However, exposure to sunlight may also cause the melanocytes to regenerate to allow the pigmentation to come back to its original color.
Treatments that aim to reverse the changes in the skin
The traditional treatment used by dermatologists is the application of corticosteroid cream.
Studies have also shown that immunomodulator creams such as Protopic and Elidel also cause repigmentation in some cases, when used with UVB narrowband treatments.
In October 1993, a scientific report was published of successfully transplanting melanocytes to vitiligo affected areas, effectively repigmenting the region. The procedure involved taking a thin layer of pigmented skin from the patient’s gluteal region. Melanocytes were then separated out to a cellular suspension that was expanded in culture. The area to be treated was then denuded with a dermabrader and the melanocytes graft applied. Between 70 and 85 percent of patients experienced nearly complete repigmentation of their skin. The longevity of the repigmentation differed from person to person.
In early 2008 scientists at King’s College London discovered that piperine, a chemical derived from black pepper, can shorten the repigmentation process in skin and reduce the UVBexposures, produces a longer lasting and more even pigmentation.
A limited 2003 study in India of 25 patients with limited and slow-spreading vitiligo given orally-taken Ginkgo biloba found it to be “fairly effective therapy for arresting the progression of the disease”. A 2008 review of natural health products found studies to generally be of poor quality but concluded that L-phenylalanine used with phototherapy, and oral Ginkgo biloba as monotherapy showed promise.
Ulltraviolet light (UVA) treatments are normally carried out in a hospital clinic. Psoralen and Ultra Violet A light (PUVA) treatment involves taking a drug which makes the skin very sensitive to light. The skin is then exposed to ultra violet A light (UVA). Treatment is required twice a week for 6-12 months or longer. PUVA may cause side effects such as ‘sunburn’ type reactions or skin freckling. Narrowband ultaviolet B (UVB) phototherapy is now used more commonly than PUVA as it is less damaging to the skin than PUVA. As with PUVA, treatment is carried out twice weekly but there is no requirement to pre-sensitise the skin and the treatment sessions are much shorter.
 Treatment to completely de-pigment the skin
Treatment to completely de-pigment the skin
In cases of extensive vitiligo the option to de-pigment the unaffected skin may be considered to render the skin an even colour. The removal of all the skin pigment is permanent and it takes about a year to complete.
