Diabetes mellitus often referred to simply as diabetes—is a condition in which the body either does not produce enough, or does not properly respond to, insulin, a hormone produced in the pancreas. Insulin enables cells to absorb glucose in order to turn it into energy. In diabetes, the body either fails to properly respond to its own insulin, does not make enough insulin, or both. This causes glucose to accumulate in the blood, often leading to various complications.
Many types of diabetes are recognized: The principal three are:
- Type 1:Results from the body’s failure to produce insulin. It is estimated that 5-10% of Americans who are diagnosed with diabetes have type 1 diabetes. Presently almost all persons with type 1 diabetes must take insulin injections.
- Type 2:Results from Insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with relative insulin deficiency. Most Americans who are diagnosed with diabetes have type 2 diabetes. Many people destined to develop type 2 diabetes spend many years in a state of Pre-Diabetes: Termed “America’s largest healthcare epidemic, pre-diabetes indicates a condition that occurs when a person’s blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. As of 2009 there are 57 million Americans who have pre-diabetes.
- Gestational Diabetes:Pregnant women who have never had diabetes before but who have high blood sugar (glucose) levels during pregnancy are said to have gestational diabetes. Gestational diabetes affects about 4% of all pregnant women. It may precede development of type 2 (or rarely type 1).
- Many other forms of diabetes mellitus are categorized separately from these. Examples include congenital diabetes due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes.
- Being obese or overweight can hike risk of type 2 diabetes by a factor of 90
- Exercising and eating a healthy diet help keep off excess weight to prevent or delay diabetes
- A myth about diabetes is that sugar causes disease; eat a balanced diet
- The American Diabetes Association recommends keeping blood sugar levels in the range of:
- 80 – 120 mg/dL before meals
- 100 – 140 mg/dL at bedtime
Management
Medications to treat diabetes include insulin and glucose-lowering pills called oral hypoglycemic drugs.
People with type 1 diabetes cannot make their own insulin. They need daily insulin injections. Insulin does not come in pill form. Injections are generally needed one to four times per day. Some people use an insulin pump. It is worn at all times and delivers a steady flow of insulin throughout the day. Other people may use a new type of inhaled insulin.
Unlike type 1 diabetes, type 2 diabetes may respond to treatment with exercise, diet, and medicines taken by mouth. There are several types of medicines used to lower blood glucose in type 2 diabetes.
Medications may be switched to insulin during pregnancy and while breastfeeding.
Regular exercise is especially important for people with diabetes. It helps with blood sugar control, weight loss, and high blood pressure. People with diabetes who exercise are less likely to experience a heart attack or stroke than those who do not exercise regularly.
Nearly 24 million Americans have diabetes; another 57 million have prediabetes, a precursor to the disease. In fact, the Centers for Disease Control and Prevention estimates that if the diabetes epidemic continues, one in three Americans will develop it in his or her lifetime.
Diabetes Management
Diet
For most Type 1 diabetics there will always be a need for insulin injections throughout their life. However, both Type 1 and Type 2 diabetics can see dramatic normalization of their blood sugars through controlling their diet, and some Type 2 diabetics can fully control the disease by dietary modification. As diabetes can lead to many other complications it is critical to maintain blood sugars as close to normal as possible and diet is the leading factor in this level of control.
The American Diabetes Association in 1994 recommended that 60-70% of caloric intake should be in the form of carbohydrates. This is somewhat controversial, with some researchers claiming that 40% is better, while others claim benefits for a high-fiber, 75% carbohydrate diet.
An article summarizing the view of the American Diabetes Association gives many recommendations and references to the research. One of the conclusions is that caloric intake must be limited to that which is necessary for maintaining a healthy weight. The methodology of the dietary therapy has attracted lots of attentions from many scientific researchers and the protocols are ranging from nutritional balancing to ambulatory diet-care.
Medication
Currently, one goal for diabetics is to avoid or minimize chronic diabetic complications, as well as to avoid acute problems of hyperglycemia or hypoglycemia. Adequate control of diabetes leads to lower risk of complications associated with unmonitored diabetes including kidney failure (requiring dialysis or transplant), blindness, heart disease and limb amputation. The most prevalent form of medication is hypoglycemic treatment through either oral hypoglycemics and/or insulin therapy. There is emerging evidence that full-blown diabetes mellitus type 2 can be evaded in those with only mildly impaired glucose tolerance.
Patients with type 1 diabetes mellitus require direct injection of insulin as their bodies cannot produce enough (or even any) insulin. As of 2010, there is no other clinically available form of insulin administration other than injection for patients with type 1: injection can be done by insulin pump, by jet injector, or any of several forms of hypodermic needle. Non-injective methods of insulin administration have been unattainable as the insulin protein breaks down in the digestive tract. There are several insulin application mechanisms under experimental development as of 2004, including a capsule that passes to the liver and delivers insulin into the bloodstream. There have also been proposed vaccines for type I using glutamic acid decarboxylase(GAD), but these are currently not being tested by the pharmaceutical companies that have sublicensed the patents to them.
For type 2 diabetics, diabetic management consists of a combination of diet, exercise, and weight loss, in any achievable combination depending on the patient. Obesity is very common in type 2 diabetes and contributes greatly to insulin resistance. Weight reduction and exercise improve tissue sensitivity to insulin and allow its proper use by target tissues. Patients who have poor diabetic control after lifestyle modifications are typically placed on oral hypoglycemics. Some Type 2 diabetics eventually fail to respond to these and must proceed to insulin therapy.
Patient education and compliance with treatment is very important in managing the disease. Improper use of medications and insulin can be very dangerous causing hypo- or hyper-glycemic episodes.
Insulin
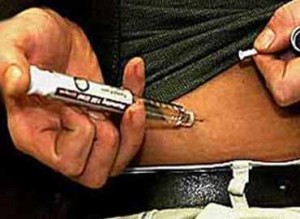 Insulin therapy requires close monitoring and a great deal of patient education, as improper administration is quite dangerous. For example, when food intake is reduced, less insulin is required. A previously satisfactory dosing may be too much if less food is consumed causing a hypoglycemic reaction if not intelligently adjusted. In addition, exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose uptake is controlled by insulin, and vice versa. In addition, there are available several types of insulin with varying times of onset and duration of action.
Insulin therapy requires close monitoring and a great deal of patient education, as improper administration is quite dangerous. For example, when food intake is reduced, less insulin is required. A previously satisfactory dosing may be too much if less food is consumed causing a hypoglycemic reaction if not intelligently adjusted. In addition, exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose uptake is controlled by insulin, and vice versa. In addition, there are available several types of insulin with varying times of onset and duration of action.
Insulin therapy creates risk because of the inability to continuously know a person’s blood glucose level and adjust insulin infusion appropriately. New advances in technology have overcome much of this problem. Small, portable insulin infusion pumps are available from several manufacturers. They allow a continuous infusion of small amounts of insulin to be delivered through the skin around the clock, plus the ability to give bolus doses when a person eats or has elevated blood glucose levels. This is very similar to how the pancreas works, but these pumps lack a continuous “feed-back” mechanism. Thus, the user is still at risk of giving too much or too little insulin unless blood glucose measurements are made. A further danger of insulin treatment is that while diabetic microangiopathy is usually explained as the result of hyperglycemia, studies in rats indicate that the higher than normal level of insulin diabetics inject to control their hyperglycemia may itself promote small blood vessel disease. While there is no clear evidence that controlling hyperglycemia reduces diabetic macrovascular and cardiovascular disease, there are indications that intensive efforts to normalize blood glucose levels may worsen cardiovascular and all-cause diabetic mortality.
The U.S. Food and Drug Administration (FDA) has approved a treatment called Exenatide, based on the saliva of a Gila monster, to control blood sugar in patients with type 2 diabetes.
